Review and Update of Intraoperative Floppy Iris Syndrome
Review Article on Recent Developments in Cataract Surgery
A narrative review of intraoperative floppy iris syndrome: an update 2020
Introduction
Intraoperative floppy iris syndrome (IFIS), first described by Chang and Campbell, is divers as a triad of intraoperative signs: billowing of a floppy iris stroma nether normal fluidics in the inductive sleeping accommodation, propensity for iris prolapse through surgical incisions, and progressive intraoperative miosis despite adequate utilise of mydriatics (1) (Figure i). IFIS primarily occurs during cataract surgery. Based on the signs observed intraoperatively, IFIS is classified into 4 grades: none (no signs), balmy (billowing simply), moderate (billowing plus either iris prolapse or progressive miosis) and severe (all the signs) (2).
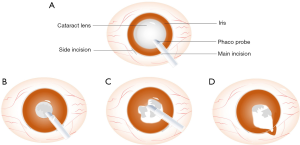
Figure ane Three characteristics of IFIS. (A) Stable status of mydriasis during a normal cataract surgery. (B,C) Three characteristics of IFIS. (B) Progressive intraoperative miosis; (C) billowing of a floppy iris stroma; (D) propensity for iris prolapse through surgical incisions. IFIS, intraoperative floppy iris syndrome.
Numerous studies accept connected tamsulosin, a selective α1 adrenoceptor adversary, with the occurrence of IFIS (1,three-6). Other potential risk factors include age, gender, race, centric length of the center, ocular comorbidities such as pseudoexfoliation syndrome and glaucoma, hypertension, diabetes mellitus, 5α-reductase inhibitors and other α adrenoceptor adversary such as silodosin, alfuzosin, doxazosin, and several neuromodulators (2,vii-12).
The occurrence of unanticipated IFIS is accompanied by increased rates of multiple complications, including corneal endothelial loss, iris trauma, inductive capsule tears, posterior capsule rupture (PCR), retained nuclear fragments, vitreous loss, macular edema and postoperative ocular inflammation (1,thirteen). These features brand IFIS an of import situation for ophthalmologists to forbid, recognize and manage appropriately. We nowadays the following article in accordance with the NARRATIVE REVIEW reporting checklist (available at http://dx.doi.org/10.21037/atm-20-3214).
Methodology
Pertinent publications were identified through a systematic search of PubMed with the following fundamental words: "intraoperative floppy iris syndrome", "cataract surgery", "phacoemulsification", "α1 adrenoceptor antagonist", and "tamsulosin". All related review articles, case reports and clinical studies were screened with no restriction on language and publication appointment. Data were extracted from each eligible article past 2 investigators working independently to analyze the ratio of IFIS in patients with α blockers including tamsulosin, terazosin, doxazosin and alfuzosin.
Give-and-take
Epidemiology
The prevalence of IFIS amid patients undergoing cataract surgery varies by populations and races. Previous data shows that the overall incidence of IFIS ranges from 2% to 3% in the United States (14) while this number is up to 12.6% in Austria (xv). Prospective observational studies evidence the incidence of IFIS is only 0.8% in Korea (sixteen) and 3.18% in China (17). About IFIS cases reported occur in patients with a medical history of using α1 adrenoceptor adversary, especially systemic tamsulosin. Tamsulosin is regarded as the first-line medical treatment for benign prostatic hyperplasia (BPH). Existing data evidence the incidence of BPH is approximately 50% in men over age 50 years, while this number increases to more lxxx% in men over their eighth decade of life (xviii). Cataract also increases with aging. The prevalence of cataract is iii.9% at age 55–64 years old while this number increases up to 92.half dozen% at age over 80 (nineteen). Surgical removal of a cataract is a standard process of choice. In industrialized countries, the connection between IFIS and tamsulosin has been largely recognized due to repeated medical educations amidst both ophthalmologists and urologists, which partially contribute to reducing the incidence of IFIS associated surgical complications post-obit specific preoperative and intraoperative interventions (xx,21). However, there withal exists a cognition gap about IFIS amid urologists based on an assessment of American urologists' knowledge of IFIS (22), indicating that continuing education is required.
Chance factors and pathogenesis
Medication
Tamsulosin, a selective α1 adrenoceptor antagonist, was establish to exist strongly associated with IFIS. It has been reported that 57–100% of patients taking tamsulosin show at to the lowest degree one classic sign of IFIS during cataract surgery (23). In addition, a meta-analysis written report reached the conclusion that odds ratio for IFIS after tamsulosin utilize was about twoscore-fold higher than that later alfuzosin employ (24).
There are three subtypes of α1 adrenoceptor including α1A, α1B and α1D. Tamsulosin mainly blocks α1A adrenoceptor, which predominantly be in prostate stromal smooth muscle, resulting in smooth musculus relaxation and subsequent relief of urinary tract symptoms (25). This particular receptor is present in iris dilator musculus as well (Figure 2). While oral tamsulosin improves the passage of urine, it results in miosis, loss of iris tone and advent of IFIS. Clinically, other α1 adrenoceptor antagonist such as doxazosin, alfuzosin and terazosin also contribute to the occurrence of IFIS (1,26-29) (Table ane). Nonetheless, the overall effect of these medicines in comparing with tamsulosin is less meaning due to their difference in receptor affinity. Besides additional technical difficulty in phaco surgery, exposure to tamsulosin inside 14 days of cataract surgery significantly increases serious postoperative complications, including loss of unabridged lens or lens fragment, retinal detachment or endophthalmitis (eleven). In that location are specific recommendations reached through survey and consensus among urologists. In short, urologists are asked to consider referring every patient with BPH for an assessment on potential cataract surgery before starting medical handling (xxx).
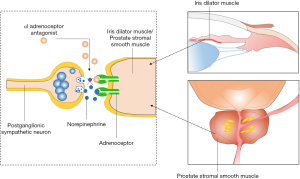
Effigy ii The mechanisms of α1 adrenoceptor antagonist on prostate and iris. α1 adrenoceptor adversary competitively binds to α1A receptors on prostate stromal and iris dilator muscle resulting relaxation of urinary tract and iris miosis.
Tamsulosin has a long one-half-life and its blocking effect to α1 adrenoceptor is irreversible. There are reports and clinical observations that IFIS can happen during cataract surgery fifty-fifty after tamsulosin therapy has been terminated years ago, which indicates that detrimental effect of tamsulosin to iris is likely permanent. An experimental written report on 20 male Wistar rats shows that iris dilator muscle layer go thinner as the duration of treatment with tamsulosin increases (31). In clinical enquiry, a cross-sectional study reveals that iris thickness at the region of dilator muscle is significantly reduced in patients receiving tamsulosin, compared to that in control group (32). This finding has been corroborated past another retrospective report (33) and a prospective report (34). Damage and atrophy to iris dilator muscle, yet, may non exist exclusively due to α1A receptor blockade. Drug-melanin interaction and consequent immune response may be underlying mechanisms as well (35). Iris vascular dysfunction may besides be related to tamsulosin handling, since α1A adrenoceptor are present inside iris arteriolar muscularis too. Investigation into the ultrastructure pathology of iris from a tamsulosin-induced IFIS patient reveals pathological changes within iris arteriolar (36). The dysfunction in iris vasculature may increase the incidence of IFIS through disturbed blood supply or structure back up (xiv). Finasteride every bit 5α-reductase inhibitors is another type of medicine prescribed for BPH, which has been suspected to cause IFIS (28). Therefore, ophthalmologists should pay attending to patients receiving finasteride likewise.
Angiotensin II receptor inhibitors are ordinarily prescribed for patients with cardiovascular diseases. Recently, a large comparative retrospective case-command written report reveals that angiotensin Two receptor inhibitors significantly contribute to the IFIS in women, which might exist an independent risk factor for the development of IFIS (37). This consequence demonstrates IFIS is not a affliction exclusive for men.
Other medications that have been reported to have increased run a risk for IFIS include neuromodulators such as onepezil, duloxetine, diazepines as well equally several antipsychotics such as chlorpromazine, quetiapine, risperidone, zuclopenthixol and aripiprazole (9,28,38-40) (Table 2). The mechanism of these drugs causing IFIS is however unknown.
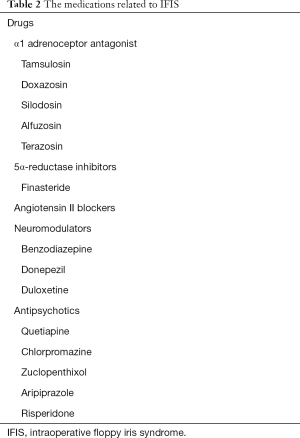
Tabular array two The medications related to IFIS
Total tableAge and gender
Although IFIS was reported during congenital cataract surgery in an infant (41), the elderly is the main patients group. Crumbling has a positive association with the incidence of IFIS (28), consistent with increased prevalence of cataract and other crumbling related degenerative diseases. Gender is some other risk factor. Many studies reveal that incidence of IFIS is significantly higher in male person than in female person (10,28). The utilize of α1 adrenoceptor adversary for men with BPH definitely increases the rate of IFIS. However, women also take this drug to treat lower urinary tract symptoms. It should be noted that the incidence of PCR was institute significantly higher in female person IFIS cases compared with male IFIS cases (10). Therefore, heart surgeons should recognize different predisposing factors among both male and female patients.
Systemic diseases and other ocular conditions
Hypertension and diabetes mellitus are 2 common diseases in the elderly. Diabetes mellitus has been reported to be unrelated to the occurrence of IFIS, while at that place are inconsistent results regarding the association of hypertension and IFIS. A report including 319 patients receiving phaco cataract surgery reveals no statistical connectedness between hypertension and IFIS (28). Notwithstanding, another prospective report consisting of one,274 cataract patients reveals hypertension as an independent risk factor for IFIS (9).
Short centric length of the eye is significantly related to IFIS through a univariate assay (9), indicating that anatomical features of ocular structure may exist a potential risk factor for IFIS. Interestingly, Wahl et al. hypothesized that longer axial length might be a cofactor for IFIS since in that location is a relatively wider space for iris stretching and different flow dynamics forcing iris movement. However, they did not detect whatsoever evidence supporting their hypothesis during their investigation (15). Shallow inductive chamber and convex iris configuration, anatomical features related to glaucoma, are predisposing factors for intraoperative iris prolapse during cataract surgery (42). However, there is no evidence that ocular comorbidities, including pseudoexfoliation syndrome and glaucoma etc., are associated with IFIS (28). Taken together, basic research and large-scale clinical studies are needed to explore the human relationship between ocular conditions and IFIS.
The management of IFIS
Preoperative evaluation
Preoperative evaluation is crucial in preventing complications associated with IFIS. Stratification and assessment of risk factors for each patient is required to determine a personalized surgical strategy (Figure 3). A comprehensive medical history should exist obtained and documented routinely before cataract surgery, especially specific medication prescription (tamsulosin and other α adrenoceptor antagonist). Once a risk cistron of IFIS is confirmed, specific surgical modifications may be proactively prepared.
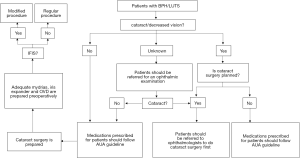
Figure 3 Flow chart recommended for urologists and ophthalmologists. BPH, benign prostatic hyperplasia; LUTS, lower urinary tract symptoms; IFIS, intraoperative floppy iris syndrome; OVD, ocular viscoelastic device; AUA, American Urological Association.
Preoperative utilize of topical atropine and epinephrine is beneficial for reducing IFIS. Epinephrine is more effective making it a ameliorate pick for patients without cardiovascular diseases (43,44). Preoperative educatee dilation should be reinforced with topical nonsteroidal Anti-inflammatory Drugs (NSAIDs), which can block cyclo-oxygenase and restrain miosis caused by prostaglandins release.
Intraoperative measures
Acceptable pupil dilation is disquisitional for phaco surgery in IFIS. One time preoperative prophylaxis is ineffective in high-risk patients or in an unanticipated occasion when IFIS occurs, modified surgical techniques are needed. The mixture of 1.0% phenylephrine and 0.3% ketorolac adding irrigation solution during surgery tin can prevent or reduce the severity of IFIS. Withal, this solution is created based on experience with Caucasian population, which may not be readily usable in other races (45). Intracameral phenylephrine can reduce iris floppiness and promote iris dilation, which can exist recommended in most cases with progressive miosis. All the same, if iris dilator musculus is severely damaged, phenylephrine may not piece of work at all. Micro-incision cataract surgery with incision less than two mm has many advantages, including stabilization of the anterior bedchamber, less trend for iris prolapse and less intraoperative tissue injury with reduced intraocular inflammation. Small incision surgery can be useful for balmy cases of IFIS, just its efficiency reduces in more astringent cases (46). Some surgeons choose to utilise modified, longer-tunnel corneal incisions for phacoemulsification cataract surgery in high-risk patients (47,48). Ocular viscoelastic devices (OVDs) are introduced to improve Phaco, which are especially useful for intraoperative miosis subsequently capsulorrhexis. OVD covers intraocular structure providing satisfactory iris stability and reserving space for pupillary devices if needed.
Other surgical pearls are helpful too. A moderate apply of viscoelastic and special attention should be paid to avert viscoelastic reaching over the pupillary margin, and seeping into posterior chamber. This is quite common in an IFIS patient due to iris and pupil floppiness. If viscoelastic accumulates within posterior chamber, information technology pushes iris forward, leading to repeated iris prolapse. When iris prolapse happens in an IFIS case, the surgeon should refrain from the natural impulse of inputting more viscoelastic inside inductive chamber to push down the iris. Instead, conscientious manipulation should be performed to release viscoelastic out of the posterior chamber. More effectively, if IFIS is highly suspected to happen through preoperative cess, a pupil dilating device should be used preemptively, which commonly includes diverse types of iris retractors and pupil expanders. An iris retractor placed 1.five–ii mm behind and beneath the main phaco incision is the best and easiest option in preventing iris prolapse in IFIS. For a pupil expander, it is preferred to be inserted through clear corneal incision (2.ii–2.8 mm), after OVD injection but before other surgical steps. Another thing to go along in mind in treatment IFIS is that phaco machine should exist set at a more than "slow motion" dynamics. Floppy iris is more stable at a low IOP, low flow, and low vacuum setting (49). Attention should be constantly paid to keep the phaco tip away from iris and pupil margin, especially in cases with severe IFIS that have very modest pupil under maximal madriatics (50).
Recommendations for urologists
A prospective trial has demonstrated that discontinuation of tamsulosin before cataract surgery can neither forbid the occurrence of IFIS nor meliorate the severity of IFIS, since the side effect of tamsulosin to iris is probably permanent (51). Every bit aging is common worldwide, more people suffer from cataract every bit well as BPH/LUTS (lower urinary tract symptoms). Therefore, there are recommendations for urologists to avert the utilise of tamsulosin when their patients are probable to receive cataract surgery in the near future (Figure 3). An assessment should be performed prior to the commencement of medical treatment to BPH to avoid the incidence of IFIS. Briefly, urologists should firstly enquire their patients if they accept been diagnosed with cataracts and if a surgery is planned for the near future (52). Secondly, for patients with decreased vision without previous ophthalmic evaluation, reference to an ophthalmologist should be recommended prior to starting long-term treatment with α1-blockers, especially tamsulosin (5). Thirdly, urologists are preferred to choose other medications such as finasteride rather than tamsulosin to treat patients with cataracts and BPH/LUTS (53). Fourthly, patients who are prescribed tamsulosin should be instructed to inform their ophthalmologists that they are taking the medicine. Almost chiefly, regular cross-talk must be built between urologists and ophthalmologists.
When patients with BPH/LUTS and mild to moderate cataract exercise not have plan to do cataract surgery soon or patients do not suffer from cataract-related vision decrease, urologists should follow American Urological Association (AUA) guideline to prescribe medicines for their patients. Patients with mild LUTS secondary to BPH are recommended for α-blocker monotherapy while patients with symptomatic prostatic enlargement only without signs of carp may exist offered a 5α-reductase inhibitor. The combination of an α blocker and a 5α-reductase inhibitor is an appropriate and constructive treatment for patients with LUTS associated with manifest prostatic enlargement (54).
Conclusions
With improvement in medical and social conditions, crumbling is now worldwide, which is associated with an increased incidence of BPH and cataract. Since IFIS has a strong association with patients taking tamsulosin, a preferred treatment to BPH, it is of paramount importance for both ophthalmologists and urologists to raise awareness of their connection. Additionally, appropriate preoperative assessment of potential risks for IFIS and respective intraoperative measures are crucial to reduce complications.
Acknowledgments
Funding: None.
Provenance and Peer Review: This article was deputed by the Guest Editor (Dr. Andrzej Grzybowski) for the serial "Recent developments in cataract surgery" published in Annals of Translational Medicine. The commodity was sent for external peer review organized by the Invitee Editor and the editorial office.
Reporting Checklist: The authors take completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-3214
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/ten.21037/atm-20-3214). The series "Recent developments in cataract surgery" was deputed by the editorial office without any funding or sponsorship. AG served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of whatever function of the piece of work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC By-NC-ND 4.0), which permits the non-commercial replication and distribution of the commodity with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). Run across: https://creativecommons.org/licenses/by-nc-nd/four.0/.
References
- Chang DF, Campbell JR. Intraoperative floppy iris syndrome associated with tamsulosin. J Cataract Refract Surg 2005;31:664-73. [Crossref] [PubMed]
- Chang DF, Campbell JR, Colin J, et al. Prospective masked comparison of intraoperative floppy iris syndrome severity with tamsulosin versus alfuzosin. Ophthalmology 2014;121:829-34. [Crossref] [PubMed]
- Tiwari A. Tamsulosin and floppy iris syndrome in benign prostatic hyperplasia patients. Adept Opin Investig Drugs 2006;15:443-half dozen. [Crossref] [PubMed]
- Brogden PR, Backhouse OC, Saldana Chiliad. Intraoperative floppy iris syndrome associated with tamsulosin. Tin Fam Physician 2007;53:1148. [PubMed]
- Chang DF, Braga-Mele R, Mamalis N, et al. Clinical experience with intraoperative floppy-iris syndrome. Results of the 2008 ASCRS fellow member survey. J Cataract Refract Surg 2008;34:1201-9. [Crossref] [PubMed]
- Lunacek A, Mohamad Al-Ali B, Radmayr C, et al. Ten years of intraoperative floppy iris syndrome in the era of blastoff-blockers. Cent European J Urol 2018;71:98-104. [PubMed]
- Ipekci T, Akin Y, Hoscan B, et al. Intraoperative floppy iris syndrome associated with silodosin. Acta Ophthalmol 2015;93:e306. [Crossref] [PubMed]
- Chatterjee South, Agrawal D. Silodosin-associated intraoperative floppy iris syndrome. Indian J Ophthalmol 2017;65:538-9. [Crossref] [PubMed]
- Chatziralli IP, Peponis V, Parikakis E, et al. Chance factors for intraoperative floppy iris syndrome: a prospective study. Eye (Lond) 2016;30:1039-44. [Crossref] [PubMed]
- Tzamalis A, Matsou A, Dermenoudi 1000, et al. The role of sexual activity in intraoperative floppy-iris syndrome. J Cataract Refract Surg 2019;45:41-7. [Crossref] [PubMed]
- Christou CD, Tsinopoulos I, Ziakas North, et al. Intraoperative Floppy Iris Syndrome: Updated Perspectives. Clin Ophthalmol 2020;14:463-71. [Crossref] [PubMed]
- Dogan Chiliad, Kutluksaman B, Keles I, et al. The Effects of Systemic Alfuzosin and Tamsulosin Hydrochloride on Choroidal Thickness and Student Diameter Sizes in Cases with Beneficial Prostatic Hyperplasia. Curr Eye Res 2017;42:1638-43. [Crossref] [PubMed]
- Storr-Paulsen A, Jorgensen JS, Norregaard JC, et al. Corneal endothelial cell changes afterwards cataract surgery in patients on systemic sympathetic alpha-1a antagonist medication (tamsulosin). Acta Ophthalmol 2014;92:359-63. [Crossref] [PubMed]
- Friedman AH. Tamsulosin and the intraoperative floppy iris syndrome. Jama 2009;301:2044-5. [Crossref] [PubMed]
- Wahl M, Tipotsch-Maca SM, Vecsei-Marlovits PV. Intraoperative floppy iris syndrome and its clan with diverse concurrent medications, bulbus length, patient historic period and gender. Graefes Arch Clin Exp Ophthalmol 2017;255:113-8. [Crossref] [PubMed]
- Lim DH, Lee MG, Chung TY, et al. Korean patients taking α1-adrenergic receptor antagonists show lower incidence of intraoperative floppy iris syndrome than western patients. Br J Ophthalmol 2014;98:479-83. [Crossref] [PubMed]
- Yu J, Yao K. Comparison of the effectiveness of 2 different pharmacologic approaches to preclude intraoperative floppy iris syndrome. International Periodical of Ophthalmology 2017;17:2126-9.
- Chughtai B, Forde JC, Thomas DD, et al. Benign prostatic hyperplasia. Nat Rev Dis Primers 2016;two:16031. [Crossref] [PubMed]
- Liu YC, Wilkins Grand, Kim T, et al. Cataracts. Lancet 2017;390:600-12. [Crossref] [PubMed]
- González Martín-Moro J, Santos Arrontes D, Martinez Silva V, et al. What urologists know most intraoperative floppy-iris syndrome. J Cataract Refract Surg 2010;36:2006-7. [Crossref] [PubMed]
- Handzel DM, Briesen Due south, Rausch South, et al. Cataract surgery in patients taking alpha-1 antagonists: know the risks, avoid the complications. Dtsch Arztebl Int 2012;109:379-84. [PubMed]
- Zhang Y, Shamie N, Daneshmand S. Cess of Urologists' Knowledge of Intraoperative Floppy Iris Syndrome. Urology 2016;97:forty-5. [Crossref] [PubMed]
- Leibovici D, Bar-Kana Y, Zadok D, et al. Clan between tamsulosin and intraoperative "floppy-iris" syndrome. Isr Med Assoc J 2009;11:45-ix. [PubMed]
- Chatziralli IP, Sergentanis TN. Risk factors for intraoperative floppy iris syndrome: a meta-analysis. Ophthalmology 2011;118:730-v. [Crossref] [PubMed]
- Wang M, Wang Ten, Zhao L, et al. Macroglia-microglia interactions via TSPO signaling regulates microglial activation in the mouse retina. J Neurosci 2014;34:3793-806. [Crossref] [PubMed]
- Chadha V, Borooah S, Tey A, et al. Floppy iris behaviour during cataract surgery: associations and variations. Br J Ophthalmol 2007;91:40-ii. [Crossref] [PubMed]
- Srinivasan S, Radomski South, Chung J, et al. Intraoperative floppy-iris syndrome during cataract surgery in men using blastoff-blockers for beneficial prostatic hypertrophy. J Cataract Refract Surg 2007;33:1826-7. [Crossref] [PubMed]
- Kaczmarek IA, Prost ME, Wasyluk J. Clinical risk factors associated with intraoperative floppy iris syndrome: a prospective study. Int Ophthalmol 2019;39:541-ix. [Crossref] [PubMed]
- Wen JQ, Hong SM, Chen YD. Risk gene analysis of IFIS in age related cataract surgery. Chinese Hospital Statistics 2018;25:176-8+82.
- Chang DF, Braga-Mele R, Mamalis Northward, et al. ASCRS White Paper: clinical review of intraoperative floppy-iris syndrome. J Cataract Refract Surg 2008;34:2153-62. [Crossref] [PubMed]
- Popescu RM, Ober C, Sevastre B, et al. Complications of cataract surgery in Wistar rats undergoing treatment with tamsulosin. Exp Ther Med 2019;17:137-46. [PubMed]
- Prata TS, Palmiero PM, Angelilli A, et al. Iris morphologic changes related to alpha(1)-adrenergic receptor antagonists implications for intraoperative floppy iris syndrome. Ophthalmology 2009;116:877-81. [Crossref] [PubMed]
- Santaella RM, Destafeno JJ, Stinnett SS, et al. The effect of alpha1-adrenergic receptor adversary tamsulosin (Flomax) on iris dilator smooth muscle anatomy. Ophthalmology 2010;117:1743-9. [Crossref] [PubMed]
- Wierzchowski T, Wilczynski G, Palenga-Pydyn D, et al. Intraoperative floppy iris syndrome - epidemiology and clinical assessment. Klin Oczna 2016;118:187-90. [PubMed]
- Goseki T, Ishikawa H, Ogasawara S, et al. Effects of tamsulosin and silodosin on isolated albino and pigmented rabbit iris dilators: possible mechanism of intraoperative floppy-iris syndrome. J Cataract Refract Surg 2012;38:1643-ix. [Crossref] [PubMed]
- Panagis L, Basile G, Friedman AH, et al. Intraoperative floppy iris syndrome: report of a case and histopathologic assay. Arch Ophthalmol 2010;128:1437-41. [Crossref] [PubMed]
- Tzamalis A, Malyugin B, Ziakas N, et al. Angiotensin receptor inhibitors as primary predisposing cistron for intraoperative floppy iris syndrome in women. J Cataract Refract Surg 2019;45:696-7. [Crossref] [PubMed]
- Bilgin B, Ilhan D, Cetinkaya A, et al. Intraoperative floppy iris syndrome associated with quetiapine. Eye (Lond) 2013;27:673. [Crossref] [PubMed]
- Matsuo Chiliad, Sano I, Ikeda Y, et al. Intraoperative floppy-iris syndrome associated with utilise of antipsychotic drugs. Tin J Ophthalmol 2016;51:294-6. [Crossref] [PubMed]
- Unal M, Yucel I, Tenlik A. Intraoperative floppy-iris syndrome associated with chronic employ of chlorpromazine. Eye (Lond) 2007;21:1241-ii. [Crossref] [PubMed]
- Wilson ME Jr, Trivedi RH, Mistr Southward. Pediatric intraoperative floppy-iris syndrome. J Cataract Refract Surg 2007;33:1325-7. [Crossref] [PubMed]
- Tint NL, Dhillon Equally, Alexander P. Management of intraoperative iris prolapse: stepwise practical approach. J Cataract Refract Surg 2012;38:1845-52. [Crossref] [PubMed]
- Esen F, Bulut AE, Toker E. Efficacy and safety of low-concentration, bisulphite-containing, intracameral epinephrine and topical atropine treatments for the prevention of intraoperative floppy iris syndrome. Cutan Ocul Toxicol 2018;37:286-90. [Crossref] [PubMed]
- Nuzzi R, Arnoffi P, Tridico F. All-time Rubber Strategy in Groups at Chance of Intraoperative Floppy Iris Syndrome Evolution: Comparison Between Atropine Instillation and Adrenaline Intracameral Injection. Open Ophthalmol J 2018;12:34-40. [Crossref] [PubMed]
- Silverstein SM, Rana VK, Stephens R, et al. Issue of phenylephrine i.0%-ketorolac 0.3% injection on tamsulosin-associated intraoperative floppy-iris syndrome. J Cataract Refract Surg 2018;44:1103-8. [Crossref] [PubMed]
- Moore SP, Goggin 1000. Intraoperative floppy iris syndrome and microincision cataract surgery. J Cataract Refract Surg 2010;36:2008. [Crossref] [PubMed]
- Armarnik Due south, Mimouni Chiliad, Rosen East, et al. Modified corneal incisions in intraoperative floppy iris syndrome (IFIS)-prone patients. Graefes Arch Clin Exp Ophthalmol 2016;254:123-7. [Crossref] [PubMed]
- Blau-Near M, Mimouni Thousand, Geffen N, et al. Modified Corneal Incisions for Cataract Surgery in Patients Treated with Tamsulosin: A Prospective Report. Curr Eye Res 2019;44:381-4. [Crossref] [PubMed]
- Keklikci U, Isen Grand, Unlu Grand, et al. Incidence, clinical findings and management of intraoperative floppy iris syndrome associated with tamsulosin. Acta Ophthalmol 2009;87:306-9. [Crossref] [PubMed]
- Lockington D, Wang Z, Qi N, et al. Modelling floppy iris syndrome and the impact of educatee size and ring devices on iris displacement. Heart (Lond) 2020. [Epub ahead of print].
- Chang DF, Osher RH, Wang L, et al. Prospective multicenter evaluation of cataract surgery in patients taking tamsulosin (Flomax). Ophthalmology 2007;114:957-64. [Crossref] [PubMed]
- Lawrentschuk North, Bylsma GW. Intraoperative 'floppy iris' syndrome and its human relationship to tamsulosin: a urologist's guide. BJU Int 2006;97:2-4. [Crossref] [PubMed]
- Flach AJ. Intraoperative floppy iris syndrome: pathophysiology, prevention, and treatment. Trans Am Ophthalmol Soc 2009;107:234-9. [PubMed]
- AUA Practice Guidelines Committee . AUA guideline on management of beneficial prostatic hyperplasia (2003). Chapter 1: Diagnosis and treatment recommendations. J Urol 2003;170:530-47. [Crossref] [PubMed]
Cite this article every bit: Yang X, Liu Z, Fan Z, Grzybowski A, Wang N. A narrative review of intraoperative floppy iris syndrome: an update 2020. Ann Transl Med 2020;8(22):1546. doi: x.21037/atm-twenty-3214
Source: https://atm.amegroups.com/article/view/50691/html
0 Response to "Review and Update of Intraoperative Floppy Iris Syndrome"
Post a Comment